Journal of Gynecological Research and Obstetrics
Ovarian Ectopic Pregnancy after Endometriomal Cyst Resection, Following In vitro Fertilization (IVF): A Rare Case Report
Afsaneh Tehranian1, Sepideh Nekuie2, Maryam Razavi1, Farahnaz Sadat Ahmadi2*
2Department of Obstetrics and Gynecology, General Dr. Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran
Cite this as
Tehranian A, Nekuie S, Razavi M, Ahmadi FS (2016) Ovarian Ectopic Pregnancy after Endometriomal Cyst Resection, Following In Vitro Fertilization (IVF): A Rare Case Report. J Gynecol Res Obstet 2(1): 051-054. DOI: 10.17352/jgro.000019Background: primary ectopic pregnancy (EP), with 0.001-0.013% incidence rate, is a very scarce obstetrical condition. Among EPs Ovarian EP is more rarely seen?
Case: We present a case of ovarian EP following In vitro fertilization in a patient with history of endometriosis and curettage. With a primary diagnosis of tubal EP, the patient underwent laparoscopy, during which ovarian pregnancy was revealed. This was later confirmed with pathological review of the specimen.
Conclusion: Ovarian EP constitutes 3% of all EPs. Diagnosis of this condition is extremely hard before surgery; therefore, laparoscopy is considered a reliable means of diagnosis. Moreover, women conceiving with IVF-embryo transfer have a higher risk of EP.
Introduction
When the embryo is implanted in any site other than the uterine cavity EP Pregnancy occurs. Neither molecular nor histological predisposing factors have been found for this condition. Yet, current available data is suggestive of the fact that a combination of impeded transport in fallopian tube and its altered environment could be a cause of EP [1,2]. Ovarian pregnancy accounts for 1 in 2000 to 1 in 60000 of pregnancies after natural conception and 0.15% of all pregnancies, whereas it constitutes about 1-3% of all EPs [3-5]. The incidence of EP has been increasing exponentially following the vast use of assisted reproductive technologies (ART) [6,7]. It is claimed that there is a 2.1-8.6% risk of EP after IVF [8,9].
Besides that, an abnormal estradiol and/or progesterone level and their ratio has been addressed as another risk factor for EP [10-12].
Clinical presentations and ultrasound findings of an ovarian pregnancy usually resemble tubal EP or a complicated ovarian cyst [13]. As preoperative diagnosis of ovarian EP is very challenging, many cases are diagnosed during surgery [13]. Although, these are oftentimes ruptured in the first trimester and since ovaries are highly vascularized organs this can lead to massive internal bleeding and subsequent hypovolemic shock [14].
In this report we are going to present a case of ovarian EP after IVF, diagnosed during laparoscopy and confirmed by pathology, in a patient with a history of curettage following abortion and surgery for cyst endometrioma of the same ovary.
Case Presentation
A 27-year-old woman gravida 2, who had one abortion, referred to infertility clinic due to secondary infertility that has lasted for 5 years. The patient underwent a curettage three years ago following her abortion. She also has undergone surgery for resecting an endometrial cyst of the right ovary one year ago.
A cycle of IVF was begun for her. After an antagonist cycle, 10 oocyte have been retrieved by puncture and three 8-cell grade 1 embryos have been freshly placed in the uterus. Four weeks after transferring the embryo, transvaginal ultrasound (TVS) was performed in which a gestational sac of about 4 mm without fetal pole and yolk sac were reported in the uterine cavity. No abnormality was reported in the adnexa. β-hCG level was 950 IU/l at this point.
One week later, TVS was performed again, which revealed no gestational sac in the uterine cavity and an endometrial thickness of 10 mm. A target like lesion was seen in the right adnexa with a gestational sac and no fetal pole. In color Doppler survey a ring of fire appearance was reported. β-hCG level at this stage was 37049 and other laboratory findings were normal.
The patient had no signs or symptoms. No abdominal tenderness was present. She did not have vaginal bleeding. For follow up she only has had routine ultrasound scans.
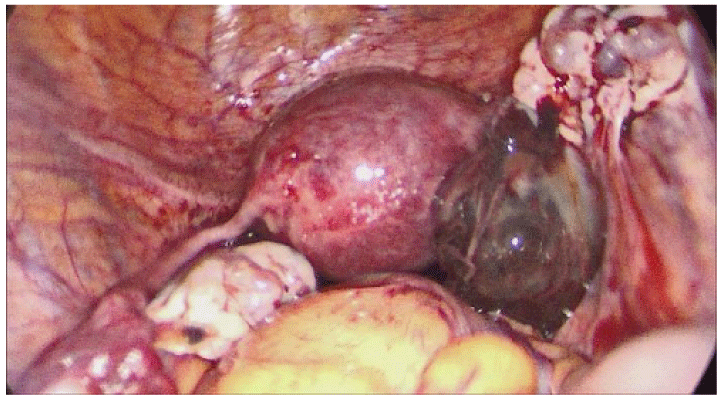
With a diagnosis of tubal EP and high β-hCG level laparoscopy was performed, during which a mild adhesion between ovaries and the posterior portion of the uterus was found. The uterus and fallopian tubes were normal. The right ovary contained a 5-cm mass with gestational products, which was resected and sent for further pathological examination (Figure 1). The pathologic report was ovarian EP with normal ovarian tissue in the wall of the gestational sac (Figures 2,3). The patient did not show any post-operative complications and her right tube and ovary were successfully preserved.
Discussion
Reported for the first time by Saint Maurice in 1682, ovarian EP is a very rare condition [15]. Moreover, its incidence is usually underestimated as it is often misdiagnosed as tubal pregnancy and is medically treated without surgical exploration and confirmation [16]. 3.2% of EPs are located in the ovaries and 1.3% in the abdomen [17]. According to an estimation by Hertig, ovarian pregnancy accounts for 1/ 25000 to 1/ 40000 of pregnancies [18].
Intrauterine contraceptive devices (IUD) are claimed to be a risk factor for EP [19], since 14-30% of patients with extra uterine EPs are said to have IUDs, while this rate for primary ovarian pregnancy is reported to be 57-90% [20-26]. One study showed the strong association between IUDs and ovarian EPs. According to this study, this association is due to the fact that IUD decreases the likelihood of uterine and tubal implantation (by 99.5% and 95% respectively), while it does not affect ovarian implantation [27-29]. Considering the 0.3% incidence rate among ART cases, these techniques have also been suggested to be a risk factor for ovarian pregnancies [13,30].
There are some theories announced, explaining possible mechanisms responsible for ovarian pregnancies: interference with the ovular release, fallopian tube functional problems and thickening of the tunica albuginea due to inflammation [31].
Ovarian pregnancies are categorized as primary and secondary. If fertilization takes place in the ovary while the egg is still in the follicle it is called primary and if fertilization happens in the tube and the conceptus is then regurgitated backwards to the ovarian stroma it is called secondary [32].
Hagit Feit et al., reported a case of ovarian EP following IVF in a patient with previous history of bilateral salpingectomy. They believe that the responsible mechanism for ovarian EP in their case was either uterine perforation with the ET catheter and implantation of the embryo on the ovary or a tuboperitoneal fistula and migration of the embryo from this fistula to the ovary [33].
In our patient many mechanisms may be responsible: ovular release impairment due to pelvic inflammation resulting from endometriosis, inflammatory thickening of tunica albuginea, or perforation of the uterus during ET. Unfortunately diagnosis of ovarian pregnancy, in most cases, is impossible before surgery; therefore, the diagnosis is usually made during surgery and with pathological examination confirmation.
In a review performed on 49 patients with ovarian EP vaginal bleeding and abdominal pain were the most frequently found symptoms. In addition, history of amenorrhea, high levels of β-bhCG, and an empty uterus on ultrasonography enhance the likelihood of ovarian EP. But it should be kept into consideration that these features are also common among other types of EP, mostly tubal EP. As ovaries are organs with great vascularization, patients with ovarian EP are at great risk of severe internal bleeding and subsequent hypovolemic shock if the ovary ruptures [35].
Comstock et al. announced an echogenic ring with small internal lucent area as the most frequently seen characteristic on the ultrasound exam [35]. Moreover, free blood or blood clots in the pelvic area are also frequent. Due to the fact that these pregnancies , mostly , have a low gestational age, a yolk sac or an embryo is very rarely identified on the ultrasound [36].
There are some important differential diagnoses, which should be kept in mind when suspecting an ovarian EP. Among these tubal EP, functional ovarian cysts, and aborted tubo-abdominal pregnancies are the crucial ones [36,37].
Preoperative diagnosis of an ovarian EP could be very challenging and is only achieved in 5.3-25% of patients [33,38]. Consequently, the definite diagnosis is only possible during operation. The Spielberg criteria, although widely accepted, is not easy to fulfill. This criteria is as follows: 1. The fallopian tube on the affected side is intact. 2. The gestational sac is located in the region of the ovary. 3. The gestational sac is attached to the uterus by the utero-ovarian ligament. 4. Ovarian tissue in the gestational sac’s wall, proved pathologically.
After the first successful laparoscopic management of ovarian pregnancy in late 1980 and early 1990, this approach has become the approach of choice and is ever since widely used [39].
The American society reproductive medicine has suggested that ovarian pregnancy should not be managed medically as the first line, but it should be diagnosed initially with surgical exploration [40]. Moreover, an array of researchers have reported failure of treatment with methotrexate; therefore, medical treatment has currently no place in management of ovarian pregnancy [34].
There is a low likelihood of recurrent ectopic pregnancy following laparoscopic resection and there is only one reported case of repeated ovarian EP up to now [41]. Koo et al., who did a research on the future outcomes of laparoscopic management, reported a 46.4% of successful intrauterine pregnancy, a 10.7% of tubal pregnancy, and a mere 3.6% of secondary infertility (one patient in their study) [34].
Conclusion
Considering the high risk of ectopic pregnancy after ART, in order to be diagnosed and managed properly, this diagnosis should be kept in mind in such patients.
- Shaw JL, Oliver E, Lee KF, Entrican G, Jabbour HN, et al. (2010) Cotinine exposure increases fallopian tube PROKR1 expression via nicotinic AChRa-7: a potential mechanism explaining the link between smoking and tubal ectopic pregnancy. Am J Pathol 177: 2509–2515.
- Goldner TE, Lawson HW, Xia Z, Atrash HK (1993) Surveillance for ectopic pregnancy—United States, 1970–1989. MMWR CDC Surveill Summ 42: 73–85.
- Tinelli A, Hudelist G, Malvasi A, Tinelli R (2008) Laparoscopic management of ovarian pregnancy. JSLS 12: 169–172.
- Scutiero G, Di Gioia P, Spada A, Greco P (2012) Primary ovarian pregnancy and its management. JSLS 16: 492-494.
- Odejinmi F, Rizzuto MI, MacRae R, Olowu O, Hussain M (2009) Diagnosis and laparoscopic management of 12 consecutive cases of ovarian pregnancy and review of literature. J Minim Invasive Gynecol 16: 354-359.
- Sivalingam VN, Duncan WC, Kirk E, Shephard LA, Horne AW (2011) Diagnosis and management of ectopic pregnancy. J Fam Plann Reprod Health Care 37: 231–240.
- Ashrafganjoei T, Nemati Honar B, Defaee S (2014) Thirteen-week ovarian pregnancy following in vitro fertilization for primary infertility treatment: a case report. Iran J Reprod Med 12: 779–784.
- Clayton HB, Schieve LA, Peterson HB, Jamieson DJ, Reynolds MA, et al. (2006) Ectopic pregnancy risk with assisted reproductive technology procedures. Obstet Gynecol 107:595-604.
- Chang HJ, Suh CS (2010) Ectopic pregnancy after assisted reproductive technology: what are the risk factors? Curr Opin Obstet Gynecol 22: 202-207.
- Paltieli Y, Eibschitz I, Ziskind G, Ohel G, Silbermann M, et al. (2000) High progesterone levels and ciliary dysfunction: a possible cause of ectopic pregnancy. J Assist Reprod Genet 17: 103-106.
- Pulkkinen MO, Jaakkola UM (1989) Low serum progesterone levels and tubal dysfunction: a possible cause of ectopic pregnancy. Am J Obstet Gynecol 161: 934-937.
- Hoover RN1, Hyer M, Pfeiffer RM, Adam E, Bond B, et al. (2011) Adverse health outcomes in women exposed in utero to diethylstilbestrol. N Engl J Med 365: 1304-1314.
- Grimes HG, Nosal RA, Gallagher JC (1983) Ovarian pregnancy: a series of 24 cases. Obstet. Gynecol 61: 174–180.
- Marcus SM, Brinsden PR (1993) Primary ovarian pregnancy after in vitro fertilization and embryo transfer: report of seven cases. Fertil Steril. 60: 167–169.
- Lurie S (1992) The history of the diagnosis and treatment of ectopic pregnancy: a medical adventure. Eur. J. Obstet Gynecol Reprod Biol 43: 1–7.
- Choi HJ, Im KS, Jung HJ, Lim KT, Mok JE, E, et al. (2011) Clinical analysis of ovarian pregnancy: a report of 49 cases. Eur. J. Obstet. Gynecol Reprod Biol 158: 87–89.
- Bouyer J, Coste J, Fernandez H, Pouly JL, Job-Spira N (2002) Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Hum Reprod 17: 3224-3230.
- Gerin-Lajoie L (1951) Ovarian pregnancy. Am J Obstet Gynecol 62: 920-929.
- Mehmood SA, Thomas JA (1985) Primary ectopic ovarian pregnancy, report of three cases. J Postgrad Med 31: 219-222.
- Ercal T, Cinar O, Mumcu A, Lacin S, Ozer E (1997) Ovarian pregnancy; relationship to an intrauterine device. Aust N Z J Obstet Gynaecol 37: 362-364.
- Bouyer J, Rachou E, Germain E, Fernandez H, Coste J, et al. (2000) Risk factors for extra uterine pregnancy in women using an intrauterine device. Fertil Steril 74: 899-908.
- Comstock C, Huston K, Lee W (2005) The ultrasonographic appearance of ovarian ectopic pregnancies. Obstet Gynecol 105: 42-45.
- Ghi T, Banfi A, Marconi R, Iaco PD, Pilu G, et al. (2005) Three dimensional sonographic diagnosis of ovarian pregnancy. Ultrasound Obstet Gynecol 26: 102-104.
- Raziel A, Golan A, Pansky M, Ron-El R, Bukovsky I, et al. (1990) Ovarian pregnancy: a report of twenty cases in one institution. Am J Obstet Gynecol 163: 1182-1185.
- Herbertsson G, Magnusson SS, Benediktsdottir K (1987) Ovarian pregnancy and IUCD use in a defined complete population. Acta Obstet Gynecol Scand 66: 607-610.
- Cabero A, Laso E, Lain JM, Manas C, Escribano I, et al. (1989) Increasing incidence of ovarian pregnancy. Eur J Obstet Gynecol Reprod Biol 31: 227-232.
- Ciortea R, Costin N, Chiroiu B, Malutan A, Mocan R, et al. (2013) Ovarian pregnancy associated with pelvic adhesions. Clujul Med 86: 77-80.
- Sandvier Sandstad E, Steir JA (1987) Ovarian pregnancy associated with intrauterine contraceptive device. Acta Obstet Gynecol Scand 66: 137-141.
- Joseph RJ, Irvine LM (2012) Ovarian ectopic pregnancy: aetiology, diagnosis, and challenges in surgical management. J Obstet Gynaecol 32: 472-474.
- Marcus SF, Brinsden PR (1995) Analysis of the incidence and risk factors associated with ectopic pregnancy following in-vitro fertilization and embryo transfer. Hum Reprod 10:199–203.
- Panda S, Darlong LM, Singh S, Borah T (2003) Case report of a primary ovarian pregnancy in aprimigravida. J Hum Reprod Sci 2: 90–92.
- Gon S, Majumdar B, Ghosal T, Sengupta M (2011) Two cases of primary ectopic ovarian pregnancies. Online J Health Allied Sci 10: 26.
- Feit H, Leibovitz Z, Kerner R, Keidar R, Sagiv R (2015) Ovarian Pregnancy Following in Vitro. Fertilization in a Woman After Bilatral Salpangectomy: A case Report and Review of the Literature. J Mini Invas Gynaecol 22: 675-677.
- Koo YJ, Choi HJ, Im KS, Jung HJ, Kwon YS (2011) Pregnancy outcomes after surgical treatment of ovarian pregnancy. Int. J. Gynecol. Obstet 114: 97–100.
- Comstock C, Huston K, Lee W (2005) The ultrasonographic appearance of ovarian ectopic pregnancies. Obstet. Gynecol 105: 42–45.
- Sergent F, Mauhger-Tinlot F, Gravier A, Verspyck E, Marpeau L (2002) Ovarian pregnancy: re-evaluation of diagnostic criteria. J Gynecol Obstet Biol 31: 742–746.
- Hallat J (1982) Primary ovarian pregnancy. A report of twenty-five cases. Am J Obstet Gynecol 143: 50–60.
- Raziel A, Schachter M, Mordechai E, Friedler S, Panski M, et al. (2004) Ovarian pregnancy – a 12-year experience of 19 cases in one institution. Eur J Obstet Gynecol Reprod Biol 114: 92–96.
- Einenkel J, Baier D, Horn LC, Alexander H, et al. (2000) Laparoscopic therapy of an intact primary ovarian pregnancy with ovarian hyper stimulation syndrome: Case report. Hum Reprod 15: 2037-2040.
- Practice Committee of the American Society for Reproductive Medicine (2006) Medical treatment of ectopic pregnancy. Fertile Steril 86: 96-102.
- Riethmuller D, Sautière JL, Benoit S, Roth P, Schaal JP, et al. (1996) [Ultrasonic diagnosis and laparoscopic treatment of an ovarian pregnancy. A case report and review of the literature]. J Gynecol Obstet Biol 25: 378–383.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
